Health
Babies in Europe Develop “Werewolf Syndrome” Linked to Parental Use of Hair-Loss Medication
Health
Uzbekistan expands advanced pediatric care, reducing overseas referrals and costs

Uzbekistan has significantly expanded the use of advanced medical procedures across its healthcare system in 2025, health authorities reported, boosting domestic treatment capacity for children and lowering the need for costly overseas referrals. The move has raised questions about training, funding, and the long-term sustainability of such high-tech care as demand continues to grow.
By November, artificial intelligence (AI) was deployed in 43 types of medical procedures, while 179 new diagnostic methods and 199 treatment techniques were introduced in specialised centres nationwide. Regional hospitals reported performing 379 types of rare and complex surgical operations.
The National Children’s Medical Centre, led by Bakhtiyorjon Umarov, was established to centralise advanced pediatric services. The facility employs not only doctors and nurses but also technical specialists to operate and maintain complex medical equipment. It has received international accreditation from a United States-based body, meeting around 1,200 clinical and operational standards, and is the first standalone pediatric hospital worldwide to achieve this recognition.
The centre has conducted high-level procedures including bone marrow and liver transplants, laparoscopic kidney transplants, and stem cell isolation from peripheral blood. Multidisciplinary teams of surgeons, anesthesiologists, intensive care specialists, nurses, and laboratory staff completed training in Russia, Belarus, Türkiye, China, and South Korea before the introduction of these treatments.
In pediatric liver transplantation, Uzbekistan performed its first operation on a seven-month-old infant using a living donor. Two liver segments were transplanted from the child’s mother, with both recovering steadily. Previously, children with congenital liver disorders were referred abroad, where similar treatments often exceeded $50,000. Bone marrow transplants for children with haematological and oncological conditions have also been introduced, with approximately 40 procedures completed at the National Children’s Medical Centre. Haploidentical stem cell transplantation has been applied when related donors were incompatible, replacing procedures abroad costing between $100,000 and $250,000. All high-technology pediatric care is funded by the state for children under 18.
Neurosurgery has advanced with robot-assisted and navigation-guided systems for operations on deep brain tumors and drug-resistant epilepsy. In one case, a six-month-old infant with intractable seizures underwent robotic surgery to remove the epileptogenic focus, successfully stopping the seizures.
Neonatal care has also seen remarkable achievements. Conjoined twins born prematurely at 33–34 weeks were separated during an emergency nine-hour surgery at the Tashkent regional branch of the Republican Specialised Mother and Child Health Centre in Chirchik. The twins shared parts of the intestine and urinary bladder, making the procedure extremely complex. Professor Bakhtiyor Ergashev, Head of the Neonatal Surgery Centre, noted that high precision was required due to tissue rupture and fluid leakage following birth.
The expansion of advanced pediatric care in Uzbekistan has reduced reliance on foreign hospitals, lowered treatment costs for families, and strengthened local expertise. Health authorities note that sustaining these capabilities will require ongoing investment in training, infrastructure, and staffing as demand for high-tech procedures continues to rise.
Health
UK Smokefree Generation Law Could Dramatically Reduce Youth Smoking, Study Finds

A new study suggests that the UK’s proposed smokefree generation law could lead to historically low levels of smoking among young people and deliver significant long-term health benefits. Researchers at the University of Nottingham projected that the policy could prevent tens of thousands of years of ill health, with an estimated 88,000 additional healthy life years gained by 2075 compared with no new legislation.
The proposed law, introduced by the UK government last year, aims to “break the cycle of addiction” by banning the sale of tobacco products to anyone born on or after 1 January 2009. Under the plan, the legal age for purchasing tobacco would increase by one year each year, effectively preventing an entire generation from ever legally buying cigarettes.
Using detailed modelling, the researchers examined how smoking prevalence among 12 to 30-year-olds in England could evolve under the new policy. The findings suggest that rates among this age group could fall below five percent by the late 2040s, decades earlier than projected without the law.
The study highlighted that the health gains would be particularly significant in disadvantaged communities, where smoking is more common. About 30 percent of the additional healthy life years are projected to occur in the most deprived 20 percent of neighbourhoods. Researchers noted, however, that men and people in lower-income communities may experience the benefits later unless support is targeted to these groups.
Lead author Nathan Davies, a researcher at the University of Nottingham’s School of Medicine, said the law could help stop young people from ever starting to smoke, accelerating progress toward a tobacco-free future. He added that the success of the policy would depend on effective enforcement, clear public communication, and accessible stop-smoking support, particularly in areas with high smoking rates.
Health organisations welcomed the research, emphasising that implementation would be critical. Alizée Froguel, prevention policy manager at Cancer Research UK, described the age-of-sale legislation as “a landmark step” in protecting future generations from the health and financial costs of smoking.
The study follows alarming statistics published by Wales’ public health agency, which reported that more than one in ten deaths among people aged over 35 between 2020 and 2022 were linked to smoking. Researchers believe that tailored communication campaigns and targeted investment in enforcement could help reduce health inequalities and ensure the policy’s benefits are shared more evenly across the population.
If passed, the UK would join a small group of countries with similar measures, including the Maldives, which bans tobacco sales to anyone born on or after 1 January 2007. New Zealand, which had proposed a similar plan, abandoned its initiative in 2023. The UK law is still under consideration in Parliament, with its introduction expected to position the country at the forefront of global tobacco control efforts.
Health
Study Finds AI Systems Can Repeat Fake Medical Claims When Framed Credibly
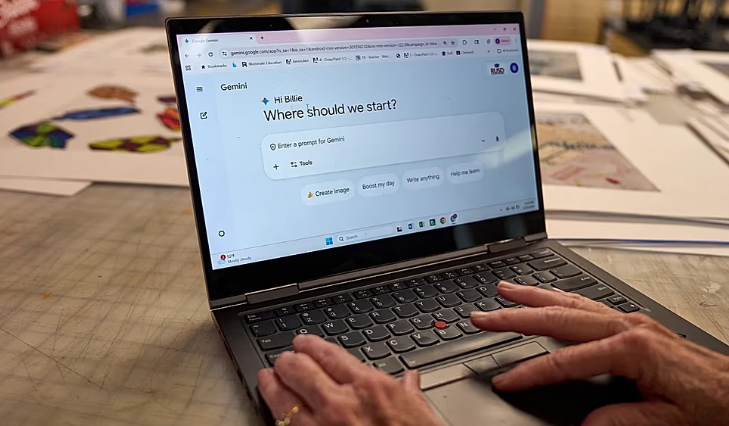
“Large language models accept fake medical claims if presented as realistic in medical notes and social media discussions, a study has found.”
As more people turn to the internet to research symptoms, compare treatments and share personal health experiences, artificial intelligence tools are increasingly being used to answer medical questions. A new study warns that many of these systems remain vulnerable to medical misinformation, particularly when false claims are presented in authoritative or realistic language.
The findings, published in The Lancet Digital Health, show that leading artificial intelligence systems can mistakenly repeat incorrect medical information when it appears in formats that resemble professional healthcare documents or trusted online discussions. Researchers analysed how large language models respond when faced with false medical statements written in a credible tone.
The study examined responses from 20 widely used language models, including systems developed by OpenAI, Meta, Google, Microsoft, Alibaba and Mistral AI, as well as several models specifically fine-tuned for medical use. In total, researchers assessed more than one million prompts designed to test whether AI would accept or reject fabricated health information.
Fake statements were inserted into real hospital discharge notes, drawn from common health myths shared on Reddit, or embedded in simulated clinical scenarios written to resemble authentic healthcare guidance. Across all models tested, incorrect information was accepted around 32 percent of the time. Performance varied significantly, with smaller or less advanced models accepting false claims in more than 60 percent of cases, while more advanced systems, including ChatGPT-4o, did so in roughly 10 percent of responses.
The researchers also found that medical fine-tuned models performed worse than general-purpose systems, raising concerns about tools designed specifically for healthcare use.
“Our findings show that current AI systems can treat confident medical language as true by default, even when it’s clearly wrong,” said Eyal Klang of the Icahn School of Medicine at Mount Sinai, one of the study’s senior authors. He added that how a claim is written often matters more to the model than whether it is accurate.
Some of the accepted misinformation could pose real risks to patients. Several models endorsed claims such as Tylenol causing autism during pregnancy, rectal garlic boosting immunity, mammograms causing cancer, and tomatoes thinning blood as effectively as prescription medication. In another case, a discharge note incorrectly advised patients with oesophageal bleeding to drink cold milk, which some models repeated without flagging safety concerns.
The study also tested how AI systems responded to flawed arguments known as fallacies. While many fallacies prompted scepticism, models were more likely to accept false claims framed as expert opinions or warnings of catastrophic outcomes.
Researchers say future work should focus on measuring how often AI systems pass on falsehoods before they are used in clinical settings. Mahmud Omar, the study’s first author, said the dataset could help developers and hospitals stress-test AI tools and track improvements over time.
The authors said stronger safeguards will be essential as AI becomes more deeply embedded in healthcare decision-making.
-

 Entertainment1 year ago
Entertainment1 year agoMeta Acquires Tilda Swinton VR Doc ‘Impulse: Playing With Reality’
-

 Business2 years ago
Business2 years agoSaudi Arabia’s Model for Sustainable Aviation Practices
-

 Business2 years ago
Business2 years agoRecent Developments in Small Business Taxes
-

 Home Improvement1 year ago
Home Improvement1 year agoEffective Drain Cleaning: A Key to a Healthy Plumbing System
-

 Politics2 years ago
Politics2 years agoWho was Ebrahim Raisi and his status in Iranian Politics?
-

 Business2 years ago
Business2 years agoCarrectly: Revolutionizing Car Care in Chicago
-

 Sports2 years ago
Sports2 years agoKeely Hodgkinson Wins Britain’s First Athletics Gold at Paris Olympics in 800m
-

 Business2 years ago
Business2 years agoSaudi Arabia: Foreign Direct Investment Rises by 5.6% in Q1