Health
Eye Diseases and the Importance of Early Prevention

Vision is one of our most essential senses, yet many take it for granted until problems arise. The eyes are intricate organs susceptible to a range of diseases that can significantly impact the quality of life if left untreated. Proactive care, including regular check-ups at an eye clinic, plays a critical role in detecting and managing potential issues early. With proper education and preventative measures, many eye conditions can be treated or avoided altogether, preserving vision for years to come.
Understanding Common Eye Diseases
- Cataracts: A cataract occurs when the lens of the eye becomes cloudy, causing blurred or dimmed vision. It is a leading cause of blindness globally, primarily affecting older adults. Risk factors include prolonged UV exposure, smoking, diabetes, and aging. Cataracts are treatable through surgical procedures that replace the cloudy lens with an artificial one. However, early detection through regular visits to an eye clinic is crucial for preventing long-term vision loss.
- Glaucoma: Often referred to as the “silent thief of sight,” glaucoma is a group of conditions that damage the optic nerve, usually due to high intraocular pressure. It progresses without symptoms in its early stages, making routine eye exams essential. Untreated glaucoma can lead to irreversible blindness, but early intervention can slow or prevent further damage.
- Macular Degeneration: This age-related condition affects the macula, the part of the retina responsible for sharp central vision. It can impair tasks such as reading and recognizing faces. While there is no cure, lifestyle changes like maintaining a diet rich in antioxidants and avoiding smoking can reduce the risk. Early detection allows for treatments like injections or laser therapy to slow progression.
- Diabetic Retinopathy: Caused by high blood sugar levels, this condition damages the blood vessels in the retina and is a leading cause of blindness among diabetics. Regular monitoring and good control of blood sugar levels can prevent or delay its onset.
The Role of Prevention in Eye Health
Prevention is the cornerstone of maintaining optimal vision and minimizing the impact of eye diseases. Early detection through routine visits to an eye clinic ensures that conditions are identified and treated before significant damage occurs. Preventative measures include:
- Healthy Diet: Consuming a diet rich in vitamins A, C, and E, as well as omega-3 fatty acids, supports eye health. Foods like spinach, kale, carrots, and fish are particularly beneficial.
- UV Protection: Prolonged exposure to ultraviolet (UV) rays can damage the eyes. Wearing sunglasses with 100% UV protection reduces this risk significantly.
- Managing Screen Time: Prolonged use of digital devices can cause eye strain. The 20-20-20 rule—taking a 20-second break to look at something 20 feet away every 20 minutes—helps alleviate discomfort.
- Quitting Smoking: Smoking increases the risk of developing cataracts, macular degeneration, and dry eye syndrome.
- Regular Check-ups: Routine visits to an eye clinic are essential, even for individuals without noticeable symptoms. Eye exams can detect conditions like glaucoma and diabetic retinopathy in their earliest stages.
Why Early Intervention Matters
Many eye diseases progress silently, making early intervention crucial for preserving vision. Advanced stages of conditions like glaucoma or diabetic retinopathy can lead to irreversible damage, underscoring the importance of regular monitoring and timely treatment. A proactive approach ensures that even subtle symptoms are addressed promptly.
The eyes are windows to the world, and protecting them should be a priority. By adopting preventative habits and staying vigilant with regular check-ups at an eye clinic, individuals can significantly reduce their risk of vision loss. Awareness, early intervention, and a commitment to eye health can ensure a lifetime of clear, vibrant sight.
Health
Drug-Resistant Superbugs Kill Thousands Across Europe, Threatening Medical Progress

Drug-resistant infections are causing more than 35,000 deaths annually across Europe, and health authorities warn the growing threat could undo years of medical progress.
Antimicrobial resistance (AMR) occurs when bacteria, viruses, and other pathogens evolve to survive existing treatments, making infections harder to treat. The resistance also increases risks for patients undergoing procedures such as organ transplants, chemotherapy, and complex surgeries.
The European Centre for Disease Prevention and Control (ECDC) released estimates on Tuesday showing that AMR contributes to tens of thousands of fatalities each year across the European Union, Iceland, Liechtenstein, and Norway. The agency described a “perfect storm” driving the rise in resistance: an ageing population more vulnerable to infections, cross-border spread of drug-resistant pathogens, overuse of antibiotics by doctors and patients, and gaps in infection prevention and control measures.
“We must ensure that no one in Europe is left without an effective treatment option,” said Dr. Diamantis Plachouras, who leads the ECDC’s work on AMR and healthcare-associated infections.
The EU Council set five targets in 2023 to combat AMR, including curbing overall antibiotic use, ensuring at least 65 per cent of antibiotics are first-line treatments, and reducing bloodstream infections from three drug-resistant bacteria. The new report shows that Europe has met only one of these goals.
Bloodstream infections caused by meticillin-resistant Staphylococcus aureus (MRSA) have fallen by 20.4 per cent since 2019, surpassing the target reduction of 15 per cent. However, new bloodstream infections from carbapenem-resistant Klebsiella pneumoniae have risen by over 60 per cent, despite a target reduction of 5 per cent. Highly resistant strains of Escherichia coli (E. coli) have also increased by more than 5 per cent, against a reduction goal of 10 per cent.
Antibiotic use across Europe has risen, including drugs meant only as last-resort treatments. This trend, combined with a shortage of new antibiotics for high-priority pathogens such as carbapenem-resistant gram-negative bacteria (CR-GNB), has left health systems struggling to keep infections under control.
ECDC Director Dr. Pamela Rendi-Wagner said urgent action is needed to curb resistance and support medical advances. “Tackling AMR requires critical innovation,” she said. She called for increased investment in promoting responsible antibiotic use, strengthening infection prevention, and developing new drugs.
Experts warn that without immediate action, Europe could face mounting deaths and rising healthcare costs. AMR is now seen not just as a clinical challenge but as a public health crisis that threatens the safety of routine medical treatments and the ability of hospitals to manage serious infections effectively.
Health
WHO Warns of Sharp Rise in Mental Health Conditions Among Europe’s Youth

A growing number of children and teenagers across Europe are experiencing mental health conditions, with global health officials warning that support systems are failing to keep pace with the surge. A new analysis released by the World Health Organization (WHO) outlines the scale of the challenge and calls for urgent action across the region.
According to the report, one in seven Europeans under the age of 20 are living with a mental health condition — a rise of about one-third over the past 15 years. The findings show clear gender disparities, with girls facing greater vulnerability. Among girls aged 15 to 19, one in four report having a mental health condition, making them the most affected group.
The report also highlights striking differences between countries. Teenagers in the Faroe Islands, Iceland and Denmark ranked among the highest for mental wellbeing, while those in Ukraine, Cyprus and Poland were placed at the lower end of the scale. The data reflects both long-term trends and the impact of recent crises.
Concerns about youth mental health have intensified in recent years, driven by a combination of social isolation, the effects of the COVID-19 pandemic, geopolitical tensions and growing economic pressures. Experts say these factors have created an environment in which young people are increasingly exposed to stress and uncertainty.
Access to professional support remains one of the region’s biggest obstacles. The WHO report notes that about one-quarter of European countries do not have community-based mental health services for young people. In addition, one in five countries lack dedicated mental health policies, leaving many children and teenagers without structured pathways to receive help.
“This report is a wake-up call,” said Dr. João Breda, who works on patient safety and healthcare quality at the WHO. “Every child and young person has the right to mental health support and high-quality care.”
The findings mark the first time the WHO has compiled extensive data on child and youth mental health across its European region, which includes 53 countries in Europe and Central Asia. The report stresses the need for stronger in-person care, noting rising concerns about young people turning to digital tools for emotional support. The document raises alarms about cases in which reliance on artificial intelligence chatbots, including ChatGPT, has led to harmful outcomes.
The WHO is urging governments to strengthen their mental health frameworks by increasing investment, expanding services and updating programmes to better reflect the needs of children and adolescents.
“By acting now, countries can build resilient systems that help the next generations thrive,” Breda said.
Health
Poliovirus Detected in Hamburg Wastewater, Raising Public Health Alerts
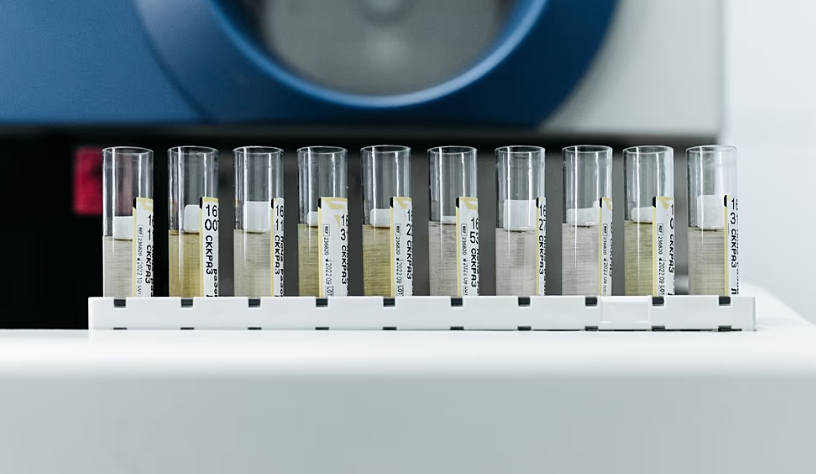
Health authorities in Germany have discovered traces of the poliovirus in sewage from Hamburg, highlighting a persistent health threat decades after Europe was declared polio-free. The finding has prompted renewed calls for enhanced disease monitoring and vaccination coverage.
Germany has not reported any confirmed cases of poliomyelitis, a highly contagious disease that primarily affects young children and can invade the nervous system, sometimes causing paralysis. The poliovirus detected in Hamburg’s wastewater is genetically similar to a strain last identified in Afghanistan, one of only two countries where polio remains endemic.
The European Centre for Disease Prevention and Control (ECDC) described the detection as “unusual, but not unexpected.” Germany’s last known locally transmitted polio case occurred in 1990, and the continent was officially declared polio-free in 2002. However, health officials caution that imported cases remain possible, particularly among populations with low vaccination coverage.
The World Health Organization (WHO) emphasized that the discovery underscores the ongoing risk: “Until polio is eradicated everywhere, all countries remain at risk of importation of the virus and potential re-infection.” Poliovirus can appear in sewage when individuals shed the virus in their stool. This does not necessarily indicate illness, as it can also result from people receiving the oral polio vaccine, which contains a weakened live virus.
Last year, similar detections in Germany, Poland, and Spain prompted health authorities to urge countries to strengthen surveillance systems and vaccination campaigns to protect populations from potential outbreaks. Across the European Union, vaccination coverage among one-year-olds ranged from 79 percent in Romania to 99 percent in Hungary and Luxembourg, according to WHO data. Experts note that gaps may persist at the local level, leaving some communities vulnerable to transmission.
Despite the presence of the virus in sewage, the ECDC stressed that the overall risk to the European population remains “very low.” Health authorities are using the findings to monitor trends and reinforce vaccination messaging, particularly in areas where immunization rates fall below recommended levels.
Germany’s recent detection serves as a reminder that polio, although rare in Europe, has not been fully eliminated globally. Public health officials continue to advocate for robust immunization programs, vigilant disease surveillance, and rapid response plans to prevent the virus from spreading should a case arise.
The Hamburg wastewater discovery has renewed focus on the importance of vaccination and monitoring, reinforcing global efforts to ensure that polio remains under control until it is eradicated worldwide.
-

 Entertainment1 year ago
Entertainment1 year agoMeta Acquires Tilda Swinton VR Doc ‘Impulse: Playing With Reality’
-

 Business1 year ago
Business1 year agoSaudi Arabia’s Model for Sustainable Aviation Practices
-

 Business1 year ago
Business1 year agoRecent Developments in Small Business Taxes
-

 Home Improvement12 months ago
Home Improvement12 months agoEffective Drain Cleaning: A Key to a Healthy Plumbing System
-

 Politics1 year ago
Politics1 year agoWho was Ebrahim Raisi and his status in Iranian Politics?
-

 Business1 year ago
Business1 year agoCarrectly: Revolutionizing Car Care in Chicago
-

 Business1 year ago
Business1 year agoSaudi Arabia: Foreign Direct Investment Rises by 5.6% in Q1
-

 Sports1 year ago
Sports1 year agoKeely Hodgkinson Wins Britain’s First Athletics Gold at Paris Olympics in 800m