Health
Ukraine’s Healthcare System Adapts and Improves Amid Ongoing Conflict
Ukraine’s healthcare system has undergone significant changes and improvements due to the ongoing impacts of Russia’s invasion, particularly for those suffering from life-altering injuries and trauma, according to Health Minister Viktor Liashko. In an exclusive interview with Euronews, Liashko emphasized the war’s influence on enhancing healthcare capabilities, notably in areas such as blood transfusions and reconstructive surgery.
Since the onset of full-scale war, Ukraine’s rehabilitation capacity has surged from 2,500 to 12,000 sessions per day. New specialized orthopedic clinics, such as the Superhumans facility in the Lviv region, are at the forefront of this transformation, serving over 3,000 patients annually with a team of more than 100 specialists. There are plans to expand operations to six regions by 2025.
A crucial aspect of the rehabilitation effort is reshaping public perceptions regarding war-related disabilities. “We are raising awareness that life does not end after losing an arm or leg,” Liashko stated, highlighting the importance of embracing artificial limbs as symbols of honor and sacrifice. “A prosthesis could symbolize that they protected their country, so they can wear them proudly.”
The minister also noted a significant shift in attitudes toward mental health, particularly for frontline soldiers and civilians under continuous stress from the conflict. “We changed the wording in our communications and started talking about mental health instead of psychiatric health to overcome stigma and encourage people to seek help,” he explained. Ukrainians face immense psychological pressure stemming from the COVID-19 pandemic and ongoing warfare, which includes constant air raids and disrupted education for children.
The government has initiated pilot projects aimed at supporting mental health among primary care doctors, teachers, and other professionals, with a focus on preventing emotional disturbances from escalating into psychiatric disorders that the health system cannot accommodate on a large scale.
As Ukraine prepares for its third winter under Russian assault, the healthcare system continues to experience stress. “There are numerous challenges that we are confident we will overcome. But the main priority today is to stop Putin,” Liashko stated.
One pressing issue remains the need for blood transfusions. To address this, Ukraine has recently launched a real-time online platform for blood donors, allowing for live updates on regional blood reserves and facilitating targeted inquiries for specific blood types.
Despite the ongoing conflict, Ukraine’s healthcare system has made strides in digital transformation, with advancements in electronic medical records and digital prescriptions. With over 35 million users and nearly 100 digital projects implemented each year, Minister Liashko asserted that, although the war has critically impacted the system, they remain committed to advancing digital solutions. “We have not stopped any digital solutions and are continuing to move forward as we did before,” he affirmed.
Health
Europe Faces Growing Challenges in Meeting Medical Care Needs, EU Report Shows

A new report has highlighted stark disparities in healthcare access across Europe, revealing that a growing number of citizens face unmet medical needs due to systemic issues such as high costs and long waiting times.
According to the latest data from Eurostat and the Health at a Glance: Europe 2024 report, 3.8 per cent of EU residents aged 16 and over reported unmet medical needs in the past year. However, the percentage climbs significantly when focusing solely on individuals who actively required healthcare services — with some countries reporting unmet needs among over 20 per cent of this group.
The causes are twofold: healthcare system barriers, including long waiting lists and treatment costs, account for 2.4 per cent of all cases, while 1.4 per cent stem from personal reasons such as fear of doctors, lack of time, or lack of knowledge about available care.
Unmet healthcare needs vary widely across the continent. Estonia tops the list within the EU, with 15.5 per cent of people reporting unmet needs, followed closely by Greece and Albania, each over 13 per cent. Even wealthier Nordic countries show surprising figures — Denmark (12.2 per cent), Finland, and Norway (over 7.5 per cent) — despite high healthcare spending. Conversely, countries such as Germany (0.5 per cent), Austria (1.3 per cent), and the Netherlands (1.4 per cent) report the lowest levels, pointing to more efficient and accessible healthcare systems.
Cost is a dominant barrier in nations like Greece and Albania, where over 9 per cent of citizens cited unaffordable care. In contrast, long waiting times are the primary issue in countries like Estonia (12 per cent) and Finland (7.5 per cent).
Income inequality also plays a major role. On average, 3.8 per cent of low-income individuals across the EU report unmet needs due to healthcare system issues — more than triple the 1.2 per cent reported by higher-income groups. In Greece, that gap is particularly wide, with 23 per cent of low-income respondents affected.
Healthcare experts say these disparities reflect more than just economic factors. Dr. Tit Albreht, President of the European Public Health Association (EUPHA), noted, “Unmet health needs arise from different reasons, including how well healthcare governance integrates services to meet population needs.”
Industry leaders, such as Tina Taube of the European Federation of Pharmaceutical Industries and Associations (EFPIA), stressed the importance of timely access to diagnosis and treatment. “Unmet needs are context-specific,” she said. “It’s not just about product availability, but also healthcare system readiness.”
Andy Powrie-Smith of EFPIA added that patients in some European countries wait up to seven times longer than others for the same treatments due to regulatory delays and varying national infrastructures.
The findings underscore the need for a more coordinated, equitable healthcare strategy across the continent, especially as Europe faces the challenges of an ageing population and increasingly complex medical technologies.
Health
Chinese Nationals Charged in U.S. with Smuggling Toxic Fungus Labeled a Potential Agroterrorism Threat
U.S. federal authorities have charged two Chinese nationals in connection with smuggling a dangerous agricultural fungus into the country, a move investigators describe as posing significant national security risks.
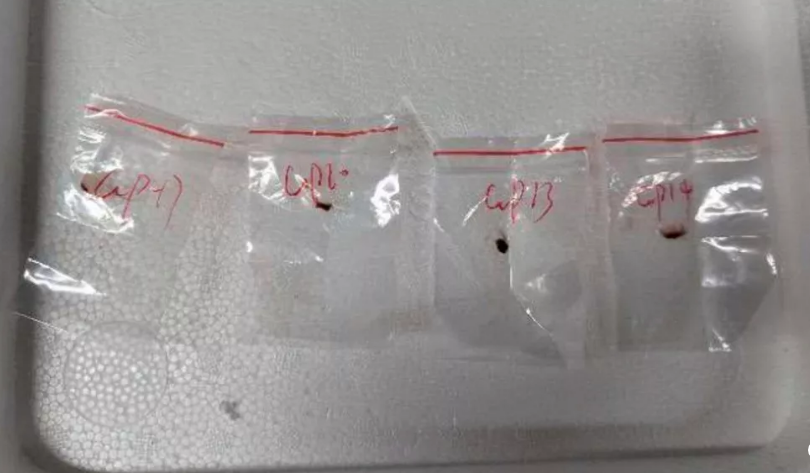
Yunqing Jian, 33, and Zunyong Liu, 34, are accused of conspiracy, smuggling, making false statements, and visa fraud after allegedly attempting to bring Fusarium graminearum — a toxic fungus capable of devastating crops and harming humans and livestock — into the United States. The case was detailed in a court filing by the Federal Bureau of Investigation (FBI) in Detroit.
The fungus, which targets essential food staples like wheat, maize, barley, and rice, is described in a scientific journal cited by the FBI as a “potential agroterrorism weapon.” Experts warn that its spread could inflict serious damage on global food security and agricultural economies.
U.S. Attorney Jerome Gorgon Jr. emphasized the seriousness of the case, stating: “The alleged actions of these Chinese nationals, including a loyal member of the Chinese Communist Party, are of the gravest national security concerns.”
Jian made her first appearance in a Detroit federal court on Tuesday and remains in custody awaiting a bond hearing scheduled for Thursday. A court-appointed attorney for her initial appearance declined to comment.
According to the FBI’s complaint, the investigation began in July 2024 when Liu was stopped at Detroit Metropolitan Airport. During a routine screening, customs officials discovered suspicious red plant material in his backpack. Liu initially claimed not to know what it was but later admitted he planned to use it for research purposes at the University of Michigan, where Jian is currently employed and where Liu previously worked.
Authorities say Liu’s mobile phone contained an article titled “Plant-Pathogen Warfare under Changing Climate Conditions,” raising further concerns about the intended use of the samples. The FBI believes the two individuals were coordinating to introduce the pathogen into a U.S. research setting without proper clearance or oversight.
Liu was denied entry to the U.S. and deported in July. Charges against both individuals were filed this week, as prosecutors continue to investigate the scope of the alleged conspiracy.
The case underscores growing concerns in the U.S. over biosecurity and potential misuse of scientific research amid rising geopolitical tensions.
Health
US Expands Measles Vaccination Guidance Amid Global Surge in Cases
-

 Business1 year ago
Business1 year agoSaudi Arabia’s Model for Sustainable Aviation Practices
-

 Business1 year ago
Business1 year agoRecent Developments in Small Business Taxes
-

 Politics1 year ago
Politics1 year agoWho was Ebrahim Raisi and his status in Iranian Politics?
-

 Business11 months ago
Business11 months agoCarrectly: Revolutionizing Car Care in Chicago
-

 Business11 months ago
Business11 months agoSaudi Arabia: Foreign Direct Investment Rises by 5.6% in Q1
-

 Technology1 year ago
Technology1 year agoComparing Apple Vision Pro and Meta Quest 3
-

 Politics1 year ago
Politics1 year agoIndonesia and Malaysia Call for Israel’s Compliance with ICJ Ruling on Gaza Offensive
-

 Sports10 months ago
Sports10 months agoKeely Hodgkinson Wins Britain’s First Athletics Gold at Paris Olympics in 800m