Health
Exercise Proven to Boost Survival and Reduce Recurrence in Colon Cancer Patients, Landmark Study Finds

Regular physical activity could become a new standard in cancer care, following results from a major international study that found structured exercise programs significantly improve survival and reduce recurrence in colon cancer patients.
The findings, presented Sunday at the American Society of Clinical Oncology’s (ASCO) annual meeting in Chicago and published in the New England Journal of Medicine, offer the strongest evidence to date linking exercise to better cancer outcomes. Researchers from Canada, the UK, Australia, Israel, and the U.S. followed 889 patients who had completed chemotherapy for treatable colon cancer.
Participants were randomly divided into two groups: one received standard health education materials on fitness and nutrition, while the other was enrolled in a three-year coaching program. Those in the exercise group met with a coach every two weeks for a year and monthly for the following two years, receiving guidance and motivation to maintain regular physical activity.
After eight years of follow-up, patients in the exercise group experienced 28% fewer cancer recurrences and 37% fewer deaths from any cause compared to the control group.
“When we saw the results, we were just astounded,” said Dr. Christopher Booth, an oncologist at Kingston Health Sciences Centre in Ontario and a study co-author. “This is a remarkably affordable intervention that helps people feel better, live longer, and keep cancer at bay.”
Dr. Jeffrey Meyerhardt, one of the lead researchers, said this is the first randomized controlled trial to show a direct causal link between exercise and cancer recurrence prevention. Previous studies had only observed correlations.
“This is about as high a quality of evidence as you can get,” said Dr. Julie Gralow, ASCO’s chief medical officer. “I love this study because it confirms what many of us in oncology have believed for years, but couldn’t yet prove.”
While the benefits are clear, minor side effects were also reported — including muscle strains — highlighting the need for guided and gradual exercise routines. Still, the impact is seen as comparable to some cancer therapies, sparking calls for exercise programs to be integrated into cancer care and covered by insurance.
For participants like 62-year-old Terri Swain-Collins of Kingston, Ontario, the program proved life-changing. “It gave me something I could do to make myself feel better,” she said, adding that the regular check-ins kept her accountable and active.
Researchers are now analyzing blood samples collected during the study to better understand how exercise biologically influences cancer outcomes, including potential links to improved insulin processing and immune function.
With these findings, experts say cancer survivors now have a powerful, evidence-based reason to stay active — and a potential lifeline to long-term health.
Health
US Expands Measles Vaccination Guidance Amid Global Surge in Cases
Health
Irish Hospital Leads Charge to Cut Nitrous Oxide Waste Amid Climate Concerns

St John’s Hospital in Limerick has become one of the first medical facilities in Ireland to take decisive action against the environmental impact of nitrous oxide emissions by deactivating its central pipeline system for the gas, long used as an anaesthetic. The move is part of a growing effort in the healthcare sector to reduce its carbon footprint and curb avoidable waste.
Nitrous oxide, commonly known as laughing gas, has been used in hospitals for decades to relieve pain and anxiety during procedures. However, studies have shown that large volumes of the gas leak into the atmosphere due to outdated infrastructure, where it can remain for up to 120 years and contribute significantly to global warming.
Dr Hugh O’Callaghan, a consultant anaesthetist at St John’s, explained that while nitrous oxide remains safe and effective for clinical use, its delivery through centralised piping systems leads to “inevitable waste.” Instead, the hospital will now use portable canisters brought directly into operating rooms, a method that reduces gas leakage and emissions.
This initiative aligns with Ireland’s national plan to cut carbon emissions from anaesthetic gases by 50% by 2030. Other hospitals across the country are expected to follow St John’s lead in the coming months, according to the Health Service Executive (HSE).
Similar steps have already been taken in parts of the United Kingdom and the Netherlands. In England, hospitals that replaced central gas systems with mobile units saw a 55% drop in monthly nitrous oxide emissions, according to the NHS. In Manchester, the switch reportedly lowered the local health trust’s overall carbon footprint by up to 5%.
“It’s not about limiting clinical care—it’s about smarter, more sustainable delivery,” said Dr Cliff Shelton, a UK anaesthetist and co-chair of the environmental committee at the Association of Anaesthetists. The group has recommended decommissioning hospital nitrous oxide pipelines across the UK and Ireland by 2027.
Healthcare professionals increasingly acknowledge their sector’s role in climate change. Globally, the health sector accounts for about 4.4% of total emissions, with the European Union responsible for 248 million metric tons of carbon dioxide annually—trailing only the United States and China.
Although nitrous oxide and other anaesthetic gases contribute significantly to this footprint, experts stress that the bulk of emissions stem from the healthcare supply chain, including pharmaceuticals and medical equipment.
Still, efforts like those at St John’s Hospital are seen as important first steps. “When we looked into this, we found we were buying 100 times more nitrous oxide than we were actually using,” said Dr Shelton. “It’s a moral imperative to address that kind of waste.”
Health
AI Tool Could Help Target Prostate Cancer Treatment, Improve Patient Outcomes
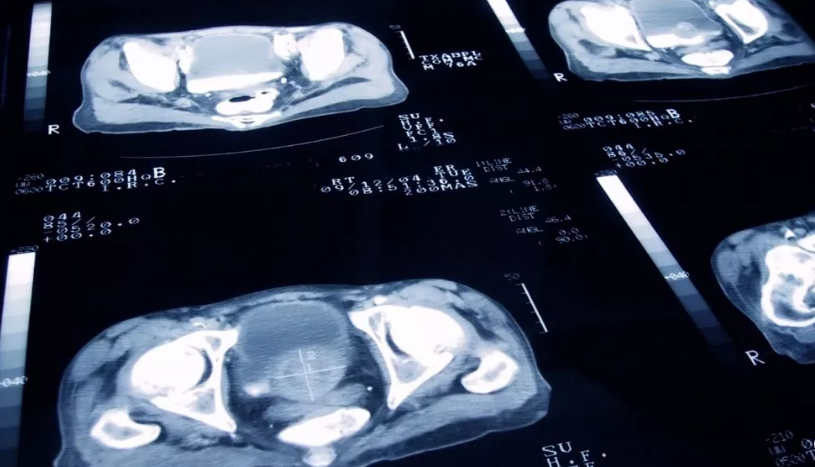
A new artificial intelligence (AI) tool could significantly improve outcomes for prostate cancer patients by identifying who would benefit most from the drug abiraterone, according to UK researchers presenting their findings at the American Society of Clinical Oncology’s annual meeting this week.
The tool analyzes tumour biopsy images to detect hidden biomarkers that predict whether a patient is likely to respond well to abiraterone, a drug known to nearly halve the risk of death for some men with prostate cancer. While effective, abiraterone is expensive and carries potential side effects such as high blood pressure, liver issues, and diabetes. These concerns have led health systems to prescribe it cautiously.
“This research shows that we can pick out the people who will respond best to abiraterone, and those who will do well from standard treatment alone – hormone therapy and radiotherapy,” said Professor Nick James, co-lead of the study from the UK’s Institute of Cancer Research.
The AI model was developed by studying tumour pathology slides and identifying molecular markers invisible to the human eye. Researchers then applied the tool to biopsy images from over 1,000 men enrolled in an earlier clinical trial on prostate cancer therapies.
Among patients whose tumours tested positive for the biomarker, abiraterone cut the five-year mortality rate from 17% to 9%. In contrast, those without the biomarker did not show a significant benefit from the drug, suggesting they could avoid unnecessary side effects and rely on standard treatments instead.
“This study shows, in a very large cohort of patients, that novel algorithms can be used to extract information from routinely available pathology slides to tailor these treatments to specific patients and minimise over-treatment whilst maximising the chance of cure,” said Professor Gert Attard of the University College London Cancer Institute, the study’s co-lead.
In the UK, access to abiraterone varies. While it is approved for use in newly diagnosed high-risk patients in Scotland and Wales, England’s NHS only offers the drug once the cancer has spread. The researchers called for policy changes, estimating that up to 8,400 men in England could benefit from earlier access.
“Access to this life-extending drug is currently a postcode lottery,” James said. “Those living in Scotland and Wales can receive the treatment for free — others cannot.”
Prostate cancer remains one of the most common cancers among men, with nearly 336,000 new cases diagnosed annually in the European Union.
-

 Business1 year ago
Business1 year agoSaudi Arabia’s Model for Sustainable Aviation Practices
-

 Business1 year ago
Business1 year agoRecent Developments in Small Business Taxes
-

 Politics1 year ago
Politics1 year agoWho was Ebrahim Raisi and his status in Iranian Politics?
-

 Business11 months ago
Business11 months agoCarrectly: Revolutionizing Car Care in Chicago
-

 Business11 months ago
Business11 months agoSaudi Arabia: Foreign Direct Investment Rises by 5.6% in Q1
-

 Technology1 year ago
Technology1 year agoComparing Apple Vision Pro and Meta Quest 3
-

 Politics1 year ago
Politics1 year agoIndonesia and Malaysia Call for Israel’s Compliance with ICJ Ruling on Gaza Offensive
-

 Sports10 months ago
Sports10 months agoKeely Hodgkinson Wins Britain’s First Athletics Gold at Paris Olympics in 800m