Health
European Medical Schools Launch Network to Train Doctors on Climate Change Health Risks
Health
Switzerland Reports First Case of Contagious New Mpox Strain as Outbreak Spreads Across Europe

Switzerland has confirmed its first case of a new, highly contagious strain of mpox, marking the latest European country to report an infection of the virus. The case, detected in a person who had recently traveled to Uganda, follows a rise in mpox infections in Central Africa, where the strain emerged in 2023.
The strain, known as clade Ib, has been responsible for thousands of infections in Central Africa, particularly in countries like Burundi and Uganda. This variant is believed to cause more severe illness, with a higher risk of death, especially among children. Health experts are also concerned that it spreads more easily than previous strains.
Mpox, a viral disease that can cause fever, headache, swollen lymph nodes, and a characteristic rash, spreads primarily through close skin-to-skin contact. In addition to the Central African region, the new strain has been detected in several countries outside of Africa, including the United States, Canada, Brazil, China, and parts of Europe.
Switzerland’s public health agency reported that the infected individual was in isolation, and no further risk to the public has been identified. However, the agency advised anyone with symptoms to seek medical advice immediately. The European Centre for Disease Prevention and Control (ECDC) confirmed the infection as part of a broader trend of rising cases in Europe linked to travel from regions experiencing active outbreaks.
The United Kingdom has also seen a number of clade Ib cases, with the most recent infection reported in April. Notably, this case was not linked to recent travel, suggesting possible local transmission. The UK Health Security Agency confirmed that no further cases were found among close contacts, and the public risk remains low. The UK has prepared for the possibility of more cases by acquiring over 150,000 doses of the mpox vaccine.
Germany has reported eight cases of the new strain, with the most recent occurring in February. Belgium and France have seen smaller numbers of cases, with infections linked to travel from Central Africa. Sweden, the first European country to report a case in 2024, remains the only nation with a confirmed infection tied to the new strain.
The World Health Organization declared a global public health emergency in August 2024, urging European health authorities to prepare for potential cases. While the risk to the general public remains low, health officials continue to monitor the situation closely, urging travelers to avoid areas with ongoing outbreaks and to seek medical advice if they develop symptoms.
As the outbreak spreads, the situation highlights the challenges of containing contagious diseases across borders, especially as global travel continues to increase.
Health
Study Reveals Surprising Global Patterns in Loneliness Among Older Adults

A major international study has uncovered significant differences in how loneliness affects older adults and those in midlife, depending on where they live. The findings challenge long-held assumptions that loneliness primarily affects the very old and very young, suggesting instead that geography, social systems, and life circumstances play key roles.
Researchers analyzed data from more than 64,000 people aged 50 to 90 across 29 countries, mostly in Europe, using a standardized loneliness scale that asked how often participants felt isolated, lacked companionship, or were left out.
The study, published in Aging & Mental Health, found that people generally become lonelier as they age. However, the extent of that loneliness varied significantly by country. In Bulgaria and Latvia, for example, older adults reported some of the steepest increases in loneliness with age, while countries like Denmark, Switzerland, and Austria reported the lowest loneliness levels overall.
Conversely, in the United States, the most pronounced loneliness was found not among the elderly but among people in midlife—making it the only country in the study where that was the case. A similar trend appeared in the Netherlands, though researchers noted data limitations there.
The study identified key factors linked to loneliness across all age groups, including unemployment, poor health, depression, and being unmarried. However, the impact of these factors varied between countries. In the U.S., for instance, being out of work in midlife was especially tied to feelings of isolation.
“Loneliness is not just a late-life issue,” said Esteban Calvo, senior author of the study and dean at Universidad Mayor in Chile. “Our findings suggest it’s influenced by a range of societal and personal factors, not just age.”
Experts say the study underscores the need for tailored, culturally sensitive approaches to addressing loneliness. “A one-size-fits-all approach will not solve this worldwide problem,” Calvo added.
The study did have limitations. Data were collected before the COVID-19 pandemic, and low response rates in some countries may affect how representative the results are. It also did not fully distinguish between different life circumstances—such as whether someone was widowed or had never married—making some findings harder to interpret.
Still, researchers say the implications are important. “Loneliness is a bit like hunger,” said Caterina Mauri, a senior researcher at the Free University of Brussels, who was not involved in the study. “It’s a signal to seek more connections, and when ignored, it can lead to serious mental and physical health consequences.”
With loneliness increasingly recognized as a global health concern, experts say more attention must be paid—not just to the elderly, but to people of all ages facing social disconnection.
Health
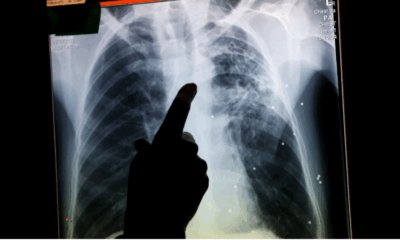
Tuberculosis Cases Surge in England as Health Officials Sound Alarm Over Resurgence

England has reported a concerning 13% increase in tuberculosis (TB) cases over the past year, marking the second consecutive annual rise and the largest jump since at least 1971. The resurgence, which affects both immigrants and people born in the UK, has prompted renewed calls for better public health strategies and improved awareness of the disease.
The UK Health Security Agency (UKHSA) confirmed 5,480 TB cases were recorded in England last year, following an 11% increase in 2022. Once thought of as a disease of the past, TB is re-emerging as a public health threat. Experts warn the spike is likely linked to disruptions in healthcare during the COVID-19 pandemic, alongside worsening social conditions such as overcrowding, homelessness, and undernutrition.
Anja Madhvani, a 35-year-old event manager from Leeds, is among those who were unexpectedly struck by the disease. While running an ultramarathon in Morocco in 2018, Madhvani became severely ill—feverish, coughing up blood, and hallucinating in the desert. Initially misdiagnosed upon returning to the UK, she was eventually found to have TB and spent nearly a year recovering through intensive treatment.
“I had been walking around with this deadly thing inside of me and had no idea,” Madhvani told Euronews Health, adding that some effects still linger. She unknowingly transmitted the disease to close contacts, including her mother, who continues to suffer health consequences years later.
TB remains the world’s deadliest infectious disease, claiming an estimated 1.25 million lives in 2023. While most prevalent in Southeast Asia and Africa, its resurgence in wealthy nations like the UK is viewed by experts as a warning sign of deeper societal issues.
“Because TB is the archetypal disease of poverty, it’s a sentinel for other conditions,” said Dr. Tom Wingfield of the Liverpool School of Tropical Medicine.
The increase has triggered a government review of its five-year TB action plan, with health officials looking to enhance early detection, improve treatment adherence, and increase screening, especially among new immigrants. However, advocates warn that funding gaps and limited mental health support for patients remain major barriers.
Despite the rise, most TB cases in the UK are not drug-resistant, meaning they are still treatable with timely medical intervention. But early diagnosis is crucial—not only to protect patients but to prevent the spread of the disease.
“I don’t think people understand what TB will do to you if you don’t get it sorted,” Madhvani said. “It doesn’t matter how wealthy you are—if you come into contact with it, you’re at risk.”
-

 Business11 months ago
Business11 months agoSaudi Arabia’s Model for Sustainable Aviation Practices
-

 Business11 months ago
Business11 months agoRecent Developments in Small Business Taxes
-

 Politics11 months ago
Politics11 months agoWho was Ebrahim Raisi and his status in Iranian Politics?
-

 Business10 months ago
Business10 months agoCarrectly: Revolutionizing Car Care in Chicago
-

 Business10 months ago
Business10 months agoSaudi Arabia: Foreign Direct Investment Rises by 5.6% in Q1
-

 Technology11 months ago
Technology11 months agoComparing Apple Vision Pro and Meta Quest 3
-

 Politics11 months ago
Politics11 months agoIndonesia and Malaysia Call for Israel’s Compliance with ICJ Ruling on Gaza Offensive
-

 Technology11 months ago
Technology11 months agoRecent Developments in AI Ethics in America