Health
Europe Pays Less for Medicines Than the U.S., but Prices Still Vary Widely by Country

Health
Exercise Proven to Boost Survival and Reduce Recurrence in Colon Cancer Patients, Landmark Study Finds

Regular physical activity could become a new standard in cancer care, following results from a major international study that found structured exercise programs significantly improve survival and reduce recurrence in colon cancer patients.
The findings, presented Sunday at the American Society of Clinical Oncology’s (ASCO) annual meeting in Chicago and published in the New England Journal of Medicine, offer the strongest evidence to date linking exercise to better cancer outcomes. Researchers from Canada, the UK, Australia, Israel, and the U.S. followed 889 patients who had completed chemotherapy for treatable colon cancer.
Participants were randomly divided into two groups: one received standard health education materials on fitness and nutrition, while the other was enrolled in a three-year coaching program. Those in the exercise group met with a coach every two weeks for a year and monthly for the following two years, receiving guidance and motivation to maintain regular physical activity.
After eight years of follow-up, patients in the exercise group experienced 28% fewer cancer recurrences and 37% fewer deaths from any cause compared to the control group.
“When we saw the results, we were just astounded,” said Dr. Christopher Booth, an oncologist at Kingston Health Sciences Centre in Ontario and a study co-author. “This is a remarkably affordable intervention that helps people feel better, live longer, and keep cancer at bay.”
Dr. Jeffrey Meyerhardt, one of the lead researchers, said this is the first randomized controlled trial to show a direct causal link between exercise and cancer recurrence prevention. Previous studies had only observed correlations.
“This is about as high a quality of evidence as you can get,” said Dr. Julie Gralow, ASCO’s chief medical officer. “I love this study because it confirms what many of us in oncology have believed for years, but couldn’t yet prove.”
While the benefits are clear, minor side effects were also reported — including muscle strains — highlighting the need for guided and gradual exercise routines. Still, the impact is seen as comparable to some cancer therapies, sparking calls for exercise programs to be integrated into cancer care and covered by insurance.
For participants like 62-year-old Terri Swain-Collins of Kingston, Ontario, the program proved life-changing. “It gave me something I could do to make myself feel better,” she said, adding that the regular check-ins kept her accountable and active.
Researchers are now analyzing blood samples collected during the study to better understand how exercise biologically influences cancer outcomes, including potential links to improved insulin processing and immune function.
With these findings, experts say cancer survivors now have a powerful, evidence-based reason to stay active — and a potential lifeline to long-term health.
Health
AI Tool Could Help Target Prostate Cancer Treatment, Improve Patient Outcomes
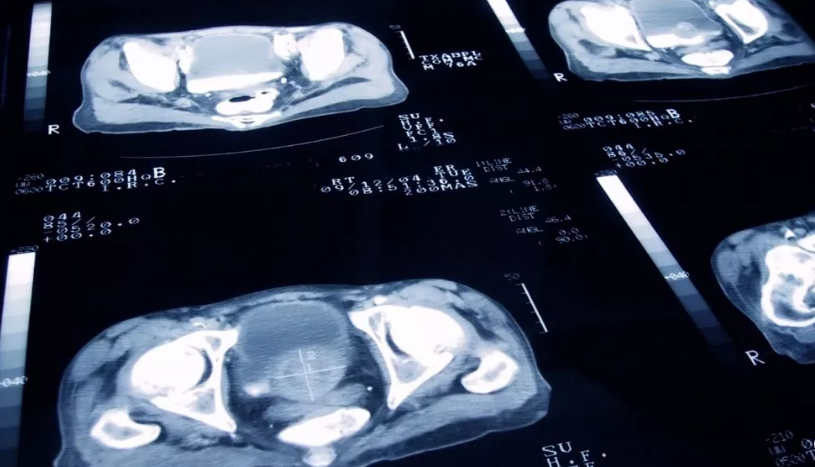
A new artificial intelligence (AI) tool could significantly improve outcomes for prostate cancer patients by identifying who would benefit most from the drug abiraterone, according to UK researchers presenting their findings at the American Society of Clinical Oncology’s annual meeting this week.
The tool analyzes tumour biopsy images to detect hidden biomarkers that predict whether a patient is likely to respond well to abiraterone, a drug known to nearly halve the risk of death for some men with prostate cancer. While effective, abiraterone is expensive and carries potential side effects such as high blood pressure, liver issues, and diabetes. These concerns have led health systems to prescribe it cautiously.
“This research shows that we can pick out the people who will respond best to abiraterone, and those who will do well from standard treatment alone – hormone therapy and radiotherapy,” said Professor Nick James, co-lead of the study from the UK’s Institute of Cancer Research.
The AI model was developed by studying tumour pathology slides and identifying molecular markers invisible to the human eye. Researchers then applied the tool to biopsy images from over 1,000 men enrolled in an earlier clinical trial on prostate cancer therapies.
Among patients whose tumours tested positive for the biomarker, abiraterone cut the five-year mortality rate from 17% to 9%. In contrast, those without the biomarker did not show a significant benefit from the drug, suggesting they could avoid unnecessary side effects and rely on standard treatments instead.
“This study shows, in a very large cohort of patients, that novel algorithms can be used to extract information from routinely available pathology slides to tailor these treatments to specific patients and minimise over-treatment whilst maximising the chance of cure,” said Professor Gert Attard of the University College London Cancer Institute, the study’s co-lead.
In the UK, access to abiraterone varies. While it is approved for use in newly diagnosed high-risk patients in Scotland and Wales, England’s NHS only offers the drug once the cancer has spread. The researchers called for policy changes, estimating that up to 8,400 men in England could benefit from earlier access.
“Access to this life-extending drug is currently a postcode lottery,” James said. “Those living in Scotland and Wales can receive the treatment for free — others cannot.”
Prostate cancer remains one of the most common cancers among men, with nearly 336,000 new cases diagnosed annually in the European Union.
Health
New Study Finds Two in Five European Teens Struggling with Mental Health, Girls Most Affected

A major new study has revealed that nearly 40% of European teenagers are experiencing poor mental well-being, with adolescent girls reporting significantly worse outcomes than boys across all 37 countries surveyed.
The findings come from the European School Survey Project on Alcohol and Other Drugs (ESPAD), which, for the first time in its 30-year history, included questions on mental health. The survey collected responses from nearly 114,000 students aged 15 and 16 across Europe.
According to the report, 59% of teens were classified as having “good mental well-being”—scoring above 50 on a standardized index measuring factors such as feeling cheerful, waking refreshed, and interest in daily life. However, the data revealed stark regional and gender disparities.
Teens in Nordic countries reported the highest levels of mental well-being, with the Faroe Islands (77%), Iceland (75%), and Denmark (72%) topping the list. In contrast, adolescents in Ukraine, still reeling from the ongoing war, ranked lowest, with only 43% reporting good mental health. Other countries with notably low scores included the Czech Republic (46%), Hungary (47%), and both Cyprus and Poland (49%).
The study highlighted that boys consistently reported better mental health than girls across all participating nations. On average, 69% of boys had good mental well-being, compared to just 49% of girls. The gap was particularly wide in countries such as Italy and Poland, where twice as many boys as girls reported feeling mentally well.
In Sweden, although overall well-being was relatively high at 62%, a closer look revealed that four in five boys reported positive mental health, while fewer than half of girls did.
Experts warn these findings point to a growing mental health crisis among Europe’s youth, intensified by social pressures, educational disruption during the COVID-19 pandemic, and the emotional toll of global conflicts and economic instability.
“Mental health is deeply connected to the broader social environments in which young people grow up,” said Kadri Soova, director of Mental Health Europe. Though not involved in the study, Soova urged policymakers to develop targeted support systems, especially for vulnerable groups like adolescent girls.
She also emphasized the importance of addressing both longstanding and emerging issues, including substance use and digital risks. “By investing in mental health education and accessible support, we can create conditions for all young people to thrive,” she said.
Mental health concerns among youth are not confined to Europe. A recent Lancet analysis found rising rates of mental health disorders among adolescents worldwide over the past decade.
-

 Business1 year ago
Business1 year agoSaudi Arabia’s Model for Sustainable Aviation Practices
-

 Business1 year ago
Business1 year agoRecent Developments in Small Business Taxes
-

 Politics1 year ago
Politics1 year agoWho was Ebrahim Raisi and his status in Iranian Politics?
-

 Business11 months ago
Business11 months agoCarrectly: Revolutionizing Car Care in Chicago
-

 Business11 months ago
Business11 months agoSaudi Arabia: Foreign Direct Investment Rises by 5.6% in Q1
-

 Technology1 year ago
Technology1 year agoComparing Apple Vision Pro and Meta Quest 3
-

 Politics1 year ago
Politics1 year agoIndonesia and Malaysia Call for Israel’s Compliance with ICJ Ruling on Gaza Offensive
-

 Sports10 months ago
Sports10 months agoKeely Hodgkinson Wins Britain’s First Athletics Gold at Paris Olympics in 800m