Health
Belgium’s Food Agency Issues Warning After Ghent Suggests Eating Christmas Trees
Health
Doctors Warn Against Over-Reliance on Online Medical Searches Amid Rise of AI Tools
Health
Semaglutide Shows Promise in Treating Serious Liver Condition, New Study Finds

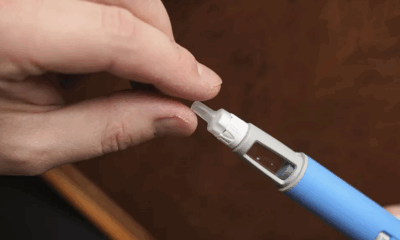
A widely used ingredient in popular weight-loss drugs has shown promising results in treating a progressive liver condition for which no medications are currently approved in the European Union, according to a major new study published in the New England Journal of Medicine.
The clinical trial, funded by Danish pharmaceutical giant Novo Nordisk, found that semaglutide – the active compound in the blockbuster drugs Ozempic and Wegovy – significantly improved outcomes for patients suffering from metabolic dysfunction-associated steatohepatitis (MASH). The disease, which causes fat accumulation, inflammation, and scarring in the liver, is associated with obesity, type 2 diabetes, and high blood pressure and can progress to cirrhosis if left untreated.
The 72-week trial involved 800 participants with MASH and moderate to advanced liver fibrosis. Patients who received weekly injections of semaglutide showed notable improvements, with 33 percent experiencing reductions in both liver inflammation and scarring, compared to just 16 percent in the placebo group. Separately, 63 percent saw a decrease in liver inflammation, and 37 percent showed improved scarring. The placebo group showed improvements of 34 percent and 22 percent, respectively.
Participants taking semaglutide also lost an average of 10.5 percent of their body weight, reinforcing the drug’s potential dual benefit in treating both liver disease and obesity-related complications.
Professor Debbie Shawcross, a liver specialist at King’s College London and vice secretary general of the European Association for the Study of the Liver, called the findings “hugely exciting,” but cautioned that semaglutide alone may not be responsible for all the improvements. Participants across both treatment arms received lifestyle counseling and support in managing related health conditions, suggesting that behavior changes also played a significant role.
“This is important as any therapy that is licensed for MASH with moderate to severe fibrosis must be used in conjunction with lifestyle interventions,” Shawcross noted.
While semaglutide showed promise, some patients reported gastrointestinal side effects, including nausea, vomiting, and diarrhea. Around 2.6 percent of those on the drug withdrew from the study due to adverse effects.
Novo Nordisk, which announced the trial’s topline results in late 2024, has stated it plans to seek regulatory approval for semaglutide as a MASH treatment in both the EU and US by mid-2025. If approved, it would become the first such therapy available in Europe.
The move comes as the EU is also reviewing other experimental treatments for MASH, including resmetirom, which was approved in the US last year after showing positive results in reducing liver scarring.
While Shawcross said it is “too early to call” semaglutide a game-changer, she emphasized its potential if used alongside comprehensive lifestyle programs. However, she warned that many patients taking weight-loss drugs do not make lasting changes, raising concerns about the long-term impact once the medication is stopped.
Health
Health Services Scramble During Widespread Blackout in Spain and Portugal

A sudden and unexplained blackout brought large parts of Spain and Portugal to a standstill on Monday, severely disrupting public services, transport, and healthcare systems across the Iberian Peninsula. With no electricity, internet, or mobile service for hours, doctors and pharmacists were forced to revert to manual methods to treat patients and protect vital medicines.
Hospitals relied on emergency generators to continue delivering essential care, including emergency surgeries and time-critical treatments. But for many family doctors, the outage meant suspending most services. At a clinic in Lisbon, Dr. Tiago Villanueva described scenes reminiscent of the early days of the COVID-19 pandemic.
“Everything stopped. We tried doing things manually, writing prescriptions by hand like it was 30 years ago,” said Villanueva, who also heads the European Union of General Practitioners. With visibility dropping as the sun set and no clear instructions from health authorities, staff eventually had no choice but to send patients home.
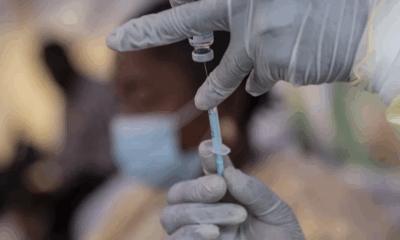
A major concern during the outage was the safety of vaccines and temperature-sensitive medicines. Power failures threatened cold-chain storage systems, putting vaccine stocks such as those for measles, tuberculosis, and other childhood diseases at risk.
Dr. João Paulo Magalhães, vice president of Portugal’s Public Health Doctors Association, warned that many vaccines may have become unusable. “Thousands of refrigerators need continuous power. Probably, there are some vaccines that are no longer viable,” he said.
In Terrassa, near Barcelona, hospital pharmacist Jordi Nicolás said his team managed to safeguard their drug inventory using hospital backup power. However, he noted that many Spanish pharmacies now rely heavily on automation. “There are a lot of robots,” said Nicolás, who is also vice president of the Spanish Society of Hospital Pharmacists. “We had to find manual workarounds to access critical medicines.”
The blackout also exposed vulnerabilities in the digital infrastructure of healthcare. Without power, pharmacists and clinics lost access to electronic medical records, making it nearly impossible to confirm prescriptions or track patient histories.
“This situation highlights the urgent need for contingency planning,” Nicolás said. Magalhães echoed the sentiment, adding that the disruption was significant and could have had serious consequences if the blackout had continued for more than a day.
While power was largely restored by late Monday evening, healthcare professionals across both countries are calling for more robust emergency systems to safeguard patient care in future crises.
“We need better ways to communicate with health authorities during events like this,” Villanueva said. “I’m even considering buying a radio — it was the only thing that worked.”
-

 Business11 months ago
Business11 months agoSaudi Arabia’s Model for Sustainable Aviation Practices
-

 Business11 months ago
Business11 months agoRecent Developments in Small Business Taxes
-

 Politics11 months ago
Politics11 months agoWho was Ebrahim Raisi and his status in Iranian Politics?
-

 Business10 months ago
Business10 months agoCarrectly: Revolutionizing Car Care in Chicago
-

 Business10 months ago
Business10 months agoSaudi Arabia: Foreign Direct Investment Rises by 5.6% in Q1
-

 Technology11 months ago
Technology11 months agoComparing Apple Vision Pro and Meta Quest 3
-

 Politics11 months ago
Politics11 months agoIndonesia and Malaysia Call for Israel’s Compliance with ICJ Ruling on Gaza Offensive
-

 Technology11 months ago
Technology11 months agoRecent Developments in AI Ethics in America