Health
EU Health Ministers Push for Critical Medicines to Be Included in Defence Funding
A coalition of 11 EU health ministers is calling for the European Union to integrate funding for critical medicines into its broader defence strategy. The proposal, outlined in an op-ed published on Euronews, urges the inclusion of the upcoming Critical Medicines Act within the EU’s new defence spending framework, citing medicine security as a crucial element of European stability.
The ministers—from Belgium, Czechia, Cyprus, Estonia, Germany, Greece, Latvia, Lithuania, Portugal, Slovenia, and Spain—argue that without a secure supply of essential medicines, Europe’s defence capabilities could be at risk.
A Call for Strategic Investment in Medicine Security
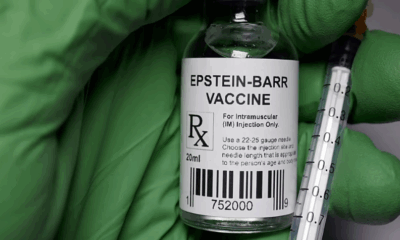
The proposed Critical Medicines Act, set to be unveiled this week by the European Commission, aims to address severe shortages of essential medicines such as antibiotics, insulin, and painkillers. The initiative would focus on medicines that are difficult to source, often relying on a limited number of manufacturers or imports from non-EU countries.
The health ministers advocate for the act to be financed under the EU’s defence budget, allowing it to access part of the €800 billion expected to be mobilized under the Rearm Europe plan. This defence funding package, discussed at last week’s extraordinary EU summit, is designed to ramp up military and security spending across the bloc.
The proposal suggests embedding medicine production investments within a new €150 billion EU defence instrument, which would enable the Commission to borrow from capital markets, issue bonds, and lend to member states.
Parallels with U.S. Defence Strategy
In their op-ed, the ministers drew comparisons to the United States’ Defence Production Act (DPA), which classifies pharmaceutical supply chains as a national security concern. The DPA allows the U.S. government to map supply chains, identify vulnerabilities, and prioritize investments in domestic pharmaceutical production.
The European ministers warn that Europe’s heavy reliance on pharmaceutical imports from Asia—where up to 80% of key medicine ingredients are sourced—poses a serious risk in times of crisis or geopolitical tensions.
“If the supply chain of antibiotics is interrupted in the midst of an escalating conflict, routine surgeries become high-risk procedures, and easily treatable infections could turn fatal,” the ministers wrote. “Foreign actors could exploit this dependency, creating a major security risk for Europe.”
Budget Implications and Political Uncertainty
The push for integrating medicine funding into defence spending comes amid uncertainty over future EU health budgets. The EU4Health programme, launched in response to the COVID-19 pandemic, received €5.3 billion in funding, but recent cuts—including the reallocation of €1 billion to aid Ukraine—have raised concerns over its sustainability.
The European Commission’s next seven-year budget is expected to be tight, and there are indications that dedicated health funding could be merged with other sectors or even eliminated. The proposed defence-linked mechanism, however, could allow increased national health spending by temporarily exempting defence-related expenditures—including medicine security—from EU fiscal limits for four years.
Will the Proposal Gain Political Backing?
It remains uncertain whether the European Commission and Members of the European Parliament (MEPs) will incorporate the ministers’ proposal into legislative talks on the Critical Medicines Act. While some policymakers may welcome a stronger pharmaceutical supply chain as part of Europe’s strategic autonomy, others may be reluctant to blur the lines between health policy and defence spending.
With the legislative proposal expected on Tuesday, the debate over how Europe secures its essential medicines is set to intensify in the coming weeks.
Health
Drug-Resistant Superbugs Kill Thousands Across Europe, Threatening Medical Progress

Drug-resistant infections are causing more than 35,000 deaths annually across Europe, and health authorities warn the growing threat could undo years of medical progress.
Antimicrobial resistance (AMR) occurs when bacteria, viruses, and other pathogens evolve to survive existing treatments, making infections harder to treat. The resistance also increases risks for patients undergoing procedures such as organ transplants, chemotherapy, and complex surgeries.
The European Centre for Disease Prevention and Control (ECDC) released estimates on Tuesday showing that AMR contributes to tens of thousands of fatalities each year across the European Union, Iceland, Liechtenstein, and Norway. The agency described a “perfect storm” driving the rise in resistance: an ageing population more vulnerable to infections, cross-border spread of drug-resistant pathogens, overuse of antibiotics by doctors and patients, and gaps in infection prevention and control measures.
“We must ensure that no one in Europe is left without an effective treatment option,” said Dr. Diamantis Plachouras, who leads the ECDC’s work on AMR and healthcare-associated infections.
The EU Council set five targets in 2023 to combat AMR, including curbing overall antibiotic use, ensuring at least 65 per cent of antibiotics are first-line treatments, and reducing bloodstream infections from three drug-resistant bacteria. The new report shows that Europe has met only one of these goals.
Bloodstream infections caused by meticillin-resistant Staphylococcus aureus (MRSA) have fallen by 20.4 per cent since 2019, surpassing the target reduction of 15 per cent. However, new bloodstream infections from carbapenem-resistant Klebsiella pneumoniae have risen by over 60 per cent, despite a target reduction of 5 per cent. Highly resistant strains of Escherichia coli (E. coli) have also increased by more than 5 per cent, against a reduction goal of 10 per cent.
Antibiotic use across Europe has risen, including drugs meant only as last-resort treatments. This trend, combined with a shortage of new antibiotics for high-priority pathogens such as carbapenem-resistant gram-negative bacteria (CR-GNB), has left health systems struggling to keep infections under control.
ECDC Director Dr. Pamela Rendi-Wagner said urgent action is needed to curb resistance and support medical advances. “Tackling AMR requires critical innovation,” she said. She called for increased investment in promoting responsible antibiotic use, strengthening infection prevention, and developing new drugs.
Experts warn that without immediate action, Europe could face mounting deaths and rising healthcare costs. AMR is now seen not just as a clinical challenge but as a public health crisis that threatens the safety of routine medical treatments and the ability of hospitals to manage serious infections effectively.
Health
WHO Warns of Sharp Rise in Mental Health Conditions Among Europe’s Youth

A growing number of children and teenagers across Europe are experiencing mental health conditions, with global health officials warning that support systems are failing to keep pace with the surge. A new analysis released by the World Health Organization (WHO) outlines the scale of the challenge and calls for urgent action across the region.
According to the report, one in seven Europeans under the age of 20 are living with a mental health condition — a rise of about one-third over the past 15 years. The findings show clear gender disparities, with girls facing greater vulnerability. Among girls aged 15 to 19, one in four report having a mental health condition, making them the most affected group.
The report also highlights striking differences between countries. Teenagers in the Faroe Islands, Iceland and Denmark ranked among the highest for mental wellbeing, while those in Ukraine, Cyprus and Poland were placed at the lower end of the scale. The data reflects both long-term trends and the impact of recent crises.
Concerns about youth mental health have intensified in recent years, driven by a combination of social isolation, the effects of the COVID-19 pandemic, geopolitical tensions and growing economic pressures. Experts say these factors have created an environment in which young people are increasingly exposed to stress and uncertainty.
Access to professional support remains one of the region’s biggest obstacles. The WHO report notes that about one-quarter of European countries do not have community-based mental health services for young people. In addition, one in five countries lack dedicated mental health policies, leaving many children and teenagers without structured pathways to receive help.
“This report is a wake-up call,” said Dr. João Breda, who works on patient safety and healthcare quality at the WHO. “Every child and young person has the right to mental health support and high-quality care.”
The findings mark the first time the WHO has compiled extensive data on child and youth mental health across its European region, which includes 53 countries in Europe and Central Asia. The report stresses the need for stronger in-person care, noting rising concerns about young people turning to digital tools for emotional support. The document raises alarms about cases in which reliance on artificial intelligence chatbots, including ChatGPT, has led to harmful outcomes.
The WHO is urging governments to strengthen their mental health frameworks by increasing investment, expanding services and updating programmes to better reflect the needs of children and adolescents.
“By acting now, countries can build resilient systems that help the next generations thrive,” Breda said.
Health
Poliovirus Detected in Hamburg Wastewater, Raising Public Health Alerts
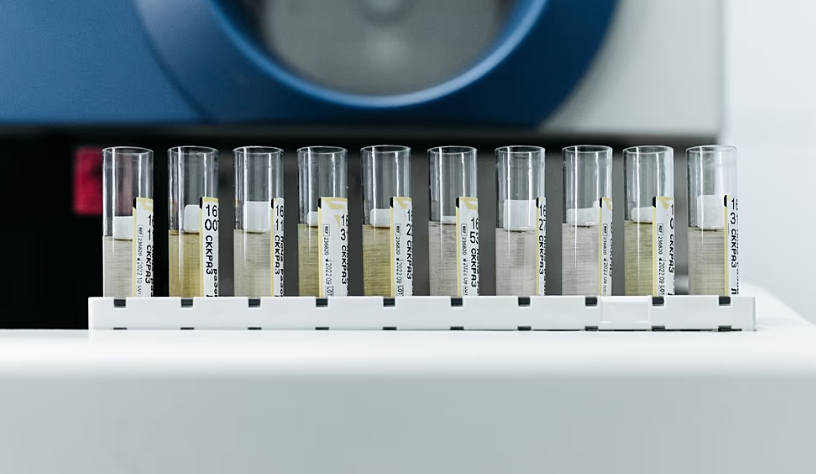
Health authorities in Germany have discovered traces of the poliovirus in sewage from Hamburg, highlighting a persistent health threat decades after Europe was declared polio-free. The finding has prompted renewed calls for enhanced disease monitoring and vaccination coverage.
Germany has not reported any confirmed cases of poliomyelitis, a highly contagious disease that primarily affects young children and can invade the nervous system, sometimes causing paralysis. The poliovirus detected in Hamburg’s wastewater is genetically similar to a strain last identified in Afghanistan, one of only two countries where polio remains endemic.
The European Centre for Disease Prevention and Control (ECDC) described the detection as “unusual, but not unexpected.” Germany’s last known locally transmitted polio case occurred in 1990, and the continent was officially declared polio-free in 2002. However, health officials caution that imported cases remain possible, particularly among populations with low vaccination coverage.
The World Health Organization (WHO) emphasized that the discovery underscores the ongoing risk: “Until polio is eradicated everywhere, all countries remain at risk of importation of the virus and potential re-infection.” Poliovirus can appear in sewage when individuals shed the virus in their stool. This does not necessarily indicate illness, as it can also result from people receiving the oral polio vaccine, which contains a weakened live virus.
Last year, similar detections in Germany, Poland, and Spain prompted health authorities to urge countries to strengthen surveillance systems and vaccination campaigns to protect populations from potential outbreaks. Across the European Union, vaccination coverage among one-year-olds ranged from 79 percent in Romania to 99 percent in Hungary and Luxembourg, according to WHO data. Experts note that gaps may persist at the local level, leaving some communities vulnerable to transmission.
Despite the presence of the virus in sewage, the ECDC stressed that the overall risk to the European population remains “very low.” Health authorities are using the findings to monitor trends and reinforce vaccination messaging, particularly in areas where immunization rates fall below recommended levels.
Germany’s recent detection serves as a reminder that polio, although rare in Europe, has not been fully eliminated globally. Public health officials continue to advocate for robust immunization programs, vigilant disease surveillance, and rapid response plans to prevent the virus from spreading should a case arise.
The Hamburg wastewater discovery has renewed focus on the importance of vaccination and monitoring, reinforcing global efforts to ensure that polio remains under control until it is eradicated worldwide.
-

 Entertainment1 year ago
Entertainment1 year agoMeta Acquires Tilda Swinton VR Doc ‘Impulse: Playing With Reality’
-

 Business1 year ago
Business1 year agoSaudi Arabia’s Model for Sustainable Aviation Practices
-

 Business1 year ago
Business1 year agoRecent Developments in Small Business Taxes
-

 Home Improvement12 months ago
Home Improvement12 months agoEffective Drain Cleaning: A Key to a Healthy Plumbing System
-

 Politics1 year ago
Politics1 year agoWho was Ebrahim Raisi and his status in Iranian Politics?
-

 Business1 year ago
Business1 year agoCarrectly: Revolutionizing Car Care in Chicago
-

 Business1 year ago
Business1 year agoSaudi Arabia: Foreign Direct Investment Rises by 5.6% in Q1
-

 Sports1 year ago
Sports1 year agoKeely Hodgkinson Wins Britain’s First Athletics Gold at Paris Olympics in 800m